Burnout in Healthcare: Rekindling the Flame of Compassionate Care
A care manager stares at her screen, the emotional weight of her last call still hanging in the air. Her patient's cancer diagnosis delivered, questions answered, tears acknowledged—now comes the aftermath. Her fingers hover over the keyboard as she navigates through multiple systems to document the conversation, capture codes, and prepare for her next call in twenty minutes. In the silence of her workspace, she must somehow process what she just experienced while racing against the clock to prepare for the next member who needs her full attention.
This moment—caught between human connection and administrative demands, between absorbing suffering and moving forward without pause—encapsulates the daily reality for healthcare professionals across the country. In this space between caring and documenting, burnout takes root.
The Silent Epidemic
Burnout in healthcare isn't new, but its recognition as a serious occupational phenomenon is. In 2019, the World Health Organization officially classified burnout in the International Classification of Diseases, acknowledging what healthcare workers had experienced for decades—a syndrome characterized by emotional exhaustion, depersonalization, and reduced personal accomplishment.
For care managers, these dimensions take on particular poignancy as they navigate complex patient needs in isolation, without the immediate support of colleagues physically present.
The Human Cost
The impact of burnout ripples outward, beginning with the care manager herself. The emotional exhaustion seeps into her home life. Sleep becomes elusive, headaches persistent. The weight of patients' suffering—their fears, losses, and pain—becomes a secondary trauma that accumulates over time. Between difficult calls, she sits alone with these burdens, with no space to process before moving to the next patient in crisis.
This suffering inevitably affects care quality. Research shows burnout correlates directly with increased errors and missed clinical cues. The therapeutic relationship suffers when emotional reserves are depleted, as patients sense the subtle withdrawal that accompanies exhaustion.
For healthcare organizations, the consequences manifest as high turnover, disrupted continuity of care, and significant recruitment costs. As experienced staff leave, those who remain shoulder heavier burdens, accelerating their own path toward burnout in a cycle that proves difficult to break.

Beyond Resilience
The healthcare industry has historically framed burnout as a personal failing requiring more "resilience." The evidence tells a different story. Burnout stems from systemic issues—administrative burden consuming up to 25% of work time, decision fatigue from hundreds of daily choices, and the profound loneliness of absorbing patient trauma without immediate colleague support.
The emotional whiplash experienced in isolation—moving from a cancer diagnosis to a medication review with no time to process—erodes even the most resilient professional over time. These systemic challenges require systemic solutions.
Reimagining Support for Healthcare Teams
The path forward requires a fundamental shift in how we support care teams. This means designing environments and tools that reduce burden rather than adding to it, that augment human capabilities instead of replacing them, and that recognize the emotional labor inherent in healthcare work.
Effective approaches must operate at multiple levels:
- Individual Level: Providing meaningful self-care resources and clear boundaries
- Team Level: Creating supportive leadership and peer connections that validate challenges
- Organizational Level: Implementing tools that reduce administrative burden and support clinical decision-making
- System Level: Advocating for policies that prioritize clinician wellbeing alongside patient outcomes
Technology as an Ally, Not Another Burden
Too often, healthcare technology has been part of the problem rather than the solution. Each new system brings promises of efficiency but delivers additional clicks, logins, and workflows that fragment attention and increase cognitive load.
However, a new generation of supportive technology is emerging—designed with deep understanding of care workflows and the unique challenges healthcare professionals face daily. These capabilities directly address the root causes of burnout with evidence-based approaches.
Evidence-Based Capabilities
Research by West et al. in The Lancet reveals that the most effective interventions combine organizational changes, workflow adjustments, and targeted support—precisely where thoughtful technology can make a difference.
Reducing Administrative Burden
Healthcare professionals currently spend up to 25% of their time on documentation. Conversation intelligence capabilities can transform this experience by automatically capturing the essence of patient interactions, organizing information into coherent clinical narratives, and eliminating manual transcription. Studies by Shanafelt confirm that reducing administrative burden constitutes one of the most effective organizational interventions for burnout.
Laguna Health - Conversation Summary: Laguna's Conversation Summary feature automatically transforms unstructured clinical conversations into comprehensive, organized clinical notes structured according to organizational preferences. After each conversation, the system produces detailed summaries including outreach context, health status, clinician actions, medication management, self-management plans, member goals, and follow-up planning. This eliminates the most time-consuming documentation task, saving hours of typing and grunt work while ensuring nothing important is missed. Care managers can focus on meaningful patient interaction rather than transcription and code selection.
Best Practice: Encourage care managers to review the generated summaries before finalizing documentation, adding any nuanced details while trusting the automated summary as a solid foundation.
Companion technology that intelligently consolidates patient information from disparate sources creates a comprehensive picture of each member in seconds rather than minutes. This capability transforms pre-call preparation from a rushed, anxiety-producing experience to a moment of focused readiness, saving valuable cognitive energy for the human interaction that follows.
Laguna Health - Case Summary and Member Profile: Laguna's Case Summary consolidates data from multiple sources into 150-200 word concise narratives that update after each interaction. These summaries highlight current health status, recent events, key social factors, barriers, and primary goals, eliminating the need for tedious scrolling through 78-page discharge summaries and re-reading previous notes across different systems. This saves 15-20 minutes of preparation time per case, allowing care managers to enter conversations fully informed and confident rather than anxious about missing critical information buried in digital files.
Best Practice: Direct care managers to read the Case Summary first before accessing any other member information, using the saved preparation time for mental readiness rather than rushing to the next task.
Breaking Through Isolation
The emotional isolation of care work—particularly when providing telephonic support—contributes significantly to burnout. Advanced conversation analysis can break through this isolation in two distinct ways:
First, by providing immediate acknowledgment of emotional labor. When a care manager handles a difficult conversation with skill and empathy, the technology notices and acknowledges these moments. This creates a "witnessed experience" that counteracts the profound loneliness of solo care work. Being seen—even by an intelligent system—helps validate the invisible emotional work that otherwise goes unrecognized.
Laguna Health - Post-Call Feedback: Laguna's Conversational Insights & Feedback system provides immediate post-call feedback that acts like having someone with you on every call. After a difficult conversation, the system might highlight how effectively you normalized a patient's emotional response or used validation techniques. It's like having a colleague say, "Hey, I know this was hard, and you were amazing!" This witnessed experience breaks through the isolation of solo care work. Organizations should encourage care managers to spend time with this feedback, using it both for acknowledgment and to see improvement opportunities. Being seen in this way is profoundly meaningful for isolated healthcare workers.
Best Practice: Encourage care managers to take a moment after each call to read their feedback, especially after difficult conversations, while supervisors reference positive feedback points during team meetings to publicly recognize excellent emotional work.
Second, by enabling meaningful human connections through supervisor insight. When care managers consistently handle challenging conversations or encounter particularly distressed members, supervisors can be automatically alerted to check in. This capability creates a human safety net for those carrying the heaviest emotional loads, ensuring timely support rather than isolation during difficult periods.
Laguna Health - Supervisor Insights: Laguna's Insights Dashboard gives supervisors visibility into team member experiences without intrusive alerts. Supervisors can review caseload complexity, identify patterns of difficult member interactions, track sentiment trends, and see which care managers are handling particularly challenging cases or encountering abusive members. This visibility enables supervisors to proactively check in, redistribute workload when needed, and provide targeted support. The dashboard creates a means for supervisors to see and help their teams carry emotional burdens rather than leaving them isolated.
Best Practice: Direct supervisors to review dashboard insights weekly to identify patterns rather than micromanage, using this data to initiate supportive conversations like "I noticed you've had several challenging interactions this week—how are you doing?"
Supporting Professional Growth
Separate from acknowledgment is the opportunity for continuous professional development. Intelligent feedback capabilities can identify specific communication patterns, empathetic responses, and effective techniques used during calls. This ongoing, personalized learning experience creates mastery over time—a factor research strongly correlates with reduced burnout rates and increased job satisfaction.
Unlike traditional training, which adds to workload, these capabilities integrate learning into the natural workflow, offering insights in the moments between calls when they're most relevant and actionable.
Laguna Health - Structured Feedback for Growth: Laguna's post-call feedback system provides specific, constructive feedback highlighting successful techniques and suggesting enhancement opportunities. This structured feedback supports professional development without additional meetings or training sessions. Research shows that constructive feedback and achievable goals significantly reduce burnout by creating a sense of mastery and progress.
Best Practice: Encourage care managers to review their feedback regularly to identify patterns in their communication strengths, while organizations create time for staff to reflect on feedback and incorporate insights into personal development plans.
Laguna Health - Supervisor Coaching Tools: The Insights Dashboard enables supervisors to structure coaching sessions based on objective data about communication strengths and improvement areas. Supervisors can identify high-performing techniques to celebrate and specific skills to develop, using conversation analytics as a foundation for meaningful professional growth discussions. This transforms coaching from subjective impressions to data-driven development opportunities that support career advancement and job satisfaction.
Best Practice: Direct supervisors to use dashboard insights when preparing for coaching sessions, focusing on specific examples of excellent communication to celebrate before addressing improvement areas, and asking open-ended questions like "I noticed you used effective validation in several calls this week—what techniques work best for you?"
Alleviating Decision Fatigue with Real-Time Intelligence
The cognitive burden of remembering details, tracking follow-up items, and prioritizing next steps across dozens of patients creates significant mental strain. Care managers make hundreds of critical decisions daily, from identifying appropriate resources to determining care priorities, often while managing emotional conversations and time pressures simultaneously.
Advanced real-time conversation analysis can now provide dynamic, contextual support precisely when care managers need it most. Rather than generic recommendations, this technology offers specific insights and suggestions tailored to the exact situation unfolding in each call, reducing the cognitive load that leads to decision fatigue.
Laguna Health - SmartPad Enhanced Real-Time Insights: Laguna's SmartPad provides dynamic real-time insights and suggestions during conversations, transforming from static recommendations to contextual, actionable support. As conversations progress, the system identifies specific member needs and surfaces relevant organizational resources, evidence-based interventions, and follow-up actions tailored to the exact situation. For example, when a caregiver mentions being overwhelmed with their own health issues while caring for a hospice patient, the system immediately suggests coordinating referrals to social workers for caregiver support. When a member expresses anxiety about procedure costs, it suggests specific financial advocacy services available through the organization. This real-time decision support works across all call types—members, family caregivers, providers, and facilities—providing care managers with intelligent assistance exactly when they need to make complex care coordination decisions. The system preserves mental energy for human judgment, empathy, and connection while ensuring no critical care opportunities are missed due to cognitive overload.
Best Practice: Train care managers to glance at real-time insights periodically during calls without interrupting their natural conversation flow, trusting their clinical judgment as insights support but never replace their expertise, with the understanding that not every suggestion needs immediate action.
Making Invisible Work Visible
Perhaps most transformative is the ability to make emotional labor visible at the organizational level. Analytics capabilities that capture and quantify the full spectrum of care—not just efficiency metrics but measures of empathy, connection, and effective support—allow organizations to recognize and value this work appropriately.
When supervisors can see the emotional complexity of cases, the effective alliance-building that prevents escalations, and the compassionate validation that supports member wellbeing, they can make more informed decisions about workload, support resources, and recognition.
Laguna Health - Comprehensive Analytics: Laguna's feedback system captures and quantifies empathy, validation, and alliance-building moments that typically go unrecognized in healthcare work. The system identifies when care managers effectively use validation techniques, build therapeutic alliance, or demonstrate exceptional empathy during difficult conversations. The Insights Dashboard presents this emotional labor alongside traditional metrics, enabling organizations to see and value the complete scope of care work. This visibility supports appropriate recognition, workload decisions, and resource allocation based on the true complexity of care management rather than just call volume or basic efficiency measures. Most importantly, this creates a sense that someone witnessed the emotional work—that the invisible labor of building trust, providing comfort, and holding space for suffering is finally seen and valued.
Best Practice: Direct supervisors to regularly acknowledge the emotional complexity captured in analytics during team meetings, using empathy and validation metrics to recognize staff during challenging periods, and incorporating these invisible work metrics into performance reviews to ensure emotional labor is valued equally with traditional productivity measures.
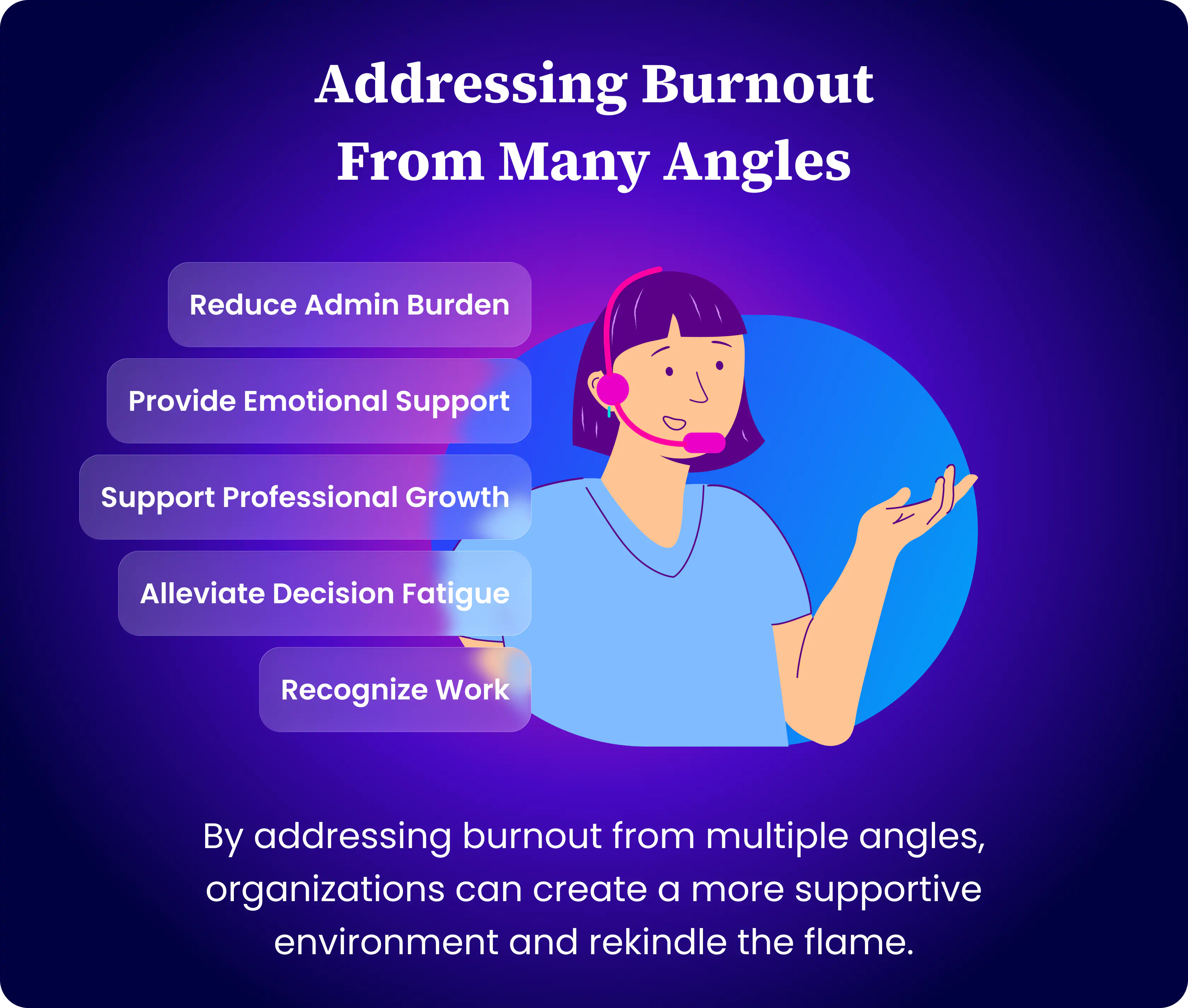
Rekindling the Flame
At day's end, our care manager finishes a call with a patient facing difficult news. She's been fully present, holding space for grief without the anxiety of documentation looming over her. Her next call preparation happens with comprehensive support, not harried searching. The weight feels lighter.
In this space—this breathing room created by thoughtful solutions—she reconnects with her purpose. The flame of compassion, nearly extinguished by systemic burdens, begins to flicker back to life.
The future of healthcare depends not just on technological innovation, but on how we use that innovation to support the humans at its heart. Because ultimately, healthcare is human work, and the technology we build should honor and enhance that humanity, not diminish it.
Get in Touch 👋
Let’s talk about how Laguna can Elevate Your Care 💜 Team


%201.webp)

