How Clinically Intelligent Conversational AI is Transforming Care Management

A Q&A with Dana Sinai, VP Conversational AI
Care management teams are essential to health plan member engagement and outcomes, but for a long time, care management has been difficult to scale efficiently. When done well, care management is highly personalized. Members are more likely to interact with care managers, and act on their recommendations, when they feel deeply understood.
So how can health plans scale care management outreach, while also ensuring that outreach is highly personalized? Many forward-thinking organizations are recognizing that clinically intelligent conversational AI may be the answer. In fact, it can help in two ways: (1) It reduces the administrative burden care management teams face (hence enabling them to reach more members), and (2) it supports highly individualized outreach that deepens member engagement and trust.
In this Q&A, Dana Sinai, VP of Conversational AI at Laguna Health, shares more about the benefits and evolution of clinically intelligent conversational AI. As a licensed clinical psychologist with nearly two decades of experience at the intersection of AI and clinical, her unique background bridges clinical practice, academic research, and data science to provide valuable insights to health plan leaders.
Q: Why is clinically intelligent AI so important, and powerful, for care management?
Dana: Conversational AI is a powerful lever for care management — if it has clinical integrity and has been developed with deep healthcare domain expertise. This is one of my top areas of focus at Laguna — bringing clinical integrity to the practical applications of data modeling and natural language processing.
For example, the call documentation we generate goes far beyond simple conversation summaries. Instead, Laguna's documentation is tailored to meet the needs and nuanced style preferences of each team while maintaining consistency and accuracy that meet the standards of each organization. For the organization that looks for the “good enough” or generic AI tools, our products may be an “overkill”. We specialize in healthcare workflows and nuance. Accordingly, the organizations we work with prioritize efficiency, quality, compliance regulations, STAR, and HEDIS ratings and they require very specific workflows, documentation and value drivers.

Q: What makes Laguna’s approach so effective?
Dana: There are several things that differentiate us. First, we train our AI with clinical expertise, which is reflected in our team structure. As a clinician who does AI work, my entire team follows this model. We work hand in hand — clinicians with data scientists, for example. Our deep domain understanding enables us to get high-grade output from our AI. We also customize our solutions to each of our customers’ unique workflows. They don't have to rely on generic solutions, because our AI adapts and adjusts to their specific style and requirements.
And, we’re focused solely on health plans, unlike many solutions that are designed for providers. Health plans have different needs and regulatory requirements. Our focus also includes the field of SDOH (Social Determinants of Health), which goes beyond pure medical factors but significantly influences health outcomes and spending.
Q: Can you share more about Laguna’s ability to incorporate SDOH information?
Dana: We extract about 50 psychological SDOH traits per member into a structured database — something unprecedented in the industry. While other databases typically contain medication, billing, and diagnosis information, Laguna also extracts structured SDOH data into each member record. We integrate these factors into our tools, assessments, documentation, and quality management tools. By providing 100% visibility into all calls and including metrics such as food security queries or any unaddressed SDOH factors, we are providing valuable information for health plans when it comes to STAR ratings, reimbursements, and bonuses.

Q: Accuracy and reliability are critical for healthcare AI applications. How does that factor into your work?
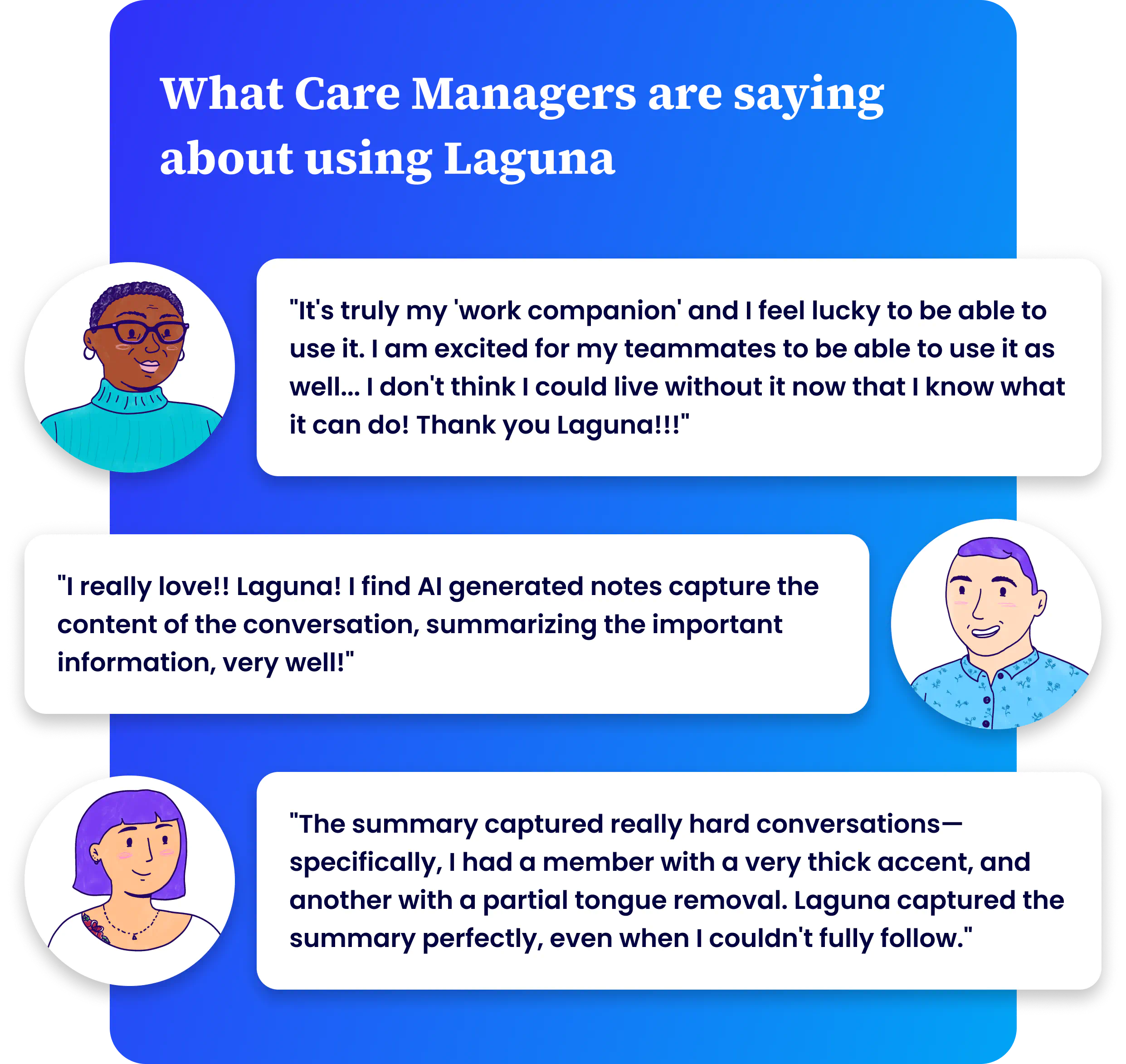
Dana: Two concepts really differentiate us at Laguna: trust and delight. First, our solution is secure, backed by evidence, accurate, and hallucination-free — attributes that build trust. Clinicians naturally begin with skepticism, but once they experience the system, they embrace it fully.
The second aspect is delight. The solution fits seamlessly into the workflow, adapts to individual needs, and creates a natural experience. Users often express that the output matches or exceeds what they would have written themselves, providing genuine support that enhances their work.
Q: What’s one other focus area for Laguna that we haven’t discussed yet, but that you are really proud of?
Dana: Our solution provides immediate feedback and opportunities for care managers’ personal development, creating a sense of learning and growth. Reduced administrative burden, immediate feedback, and personal development have been identified as significant buffers against burnout in healthcare, an industry that is known for its significant challenges in that area.
Q: What does the future hold for AI and care management?
Dana: At Laguna, we're progressing at the speed of trust. Our customers' trust is our northstar, rather than industry hype or tech buzz. This north start helps confidently bridge between the present workflow and technology realities of our customer and the possibilities unlocked by AI.
In the future, AI will free up health plans more and more to build the connections between members and care managers that make an even bigger impact.
We pride ourselves on our clinical approach, and our ability to help plans present themselves to their members not just as an insurance company, but as an organization that cares about them and knows them personally.

Learn more about how Laguna Health can support your care management team here.
Get in Touch 👋
Let’s talk about how Laguna can Elevate Your Care 💜 Team




