
Multi-State Health Plan Cuts Care Manager Documentation Time 66%, While Improving Care Quality

,
Challenge
Care managers at a multi-state health plan were spending up to 75% of their time on administrative work such as preparing for calls, taking notes, and writing summaries—which limited their direct interaction time with members.
Team supervisors had to spend hours manually reviewing calls for compliance and performance monitoring, all while the health plan was under pressure to cut administrative costs. The leadership team was looking for solutions to improve care management efficiency and quality without increasing expenses.
Solution
To address their efficiency challenges, the health plan's leadership implemented Laguna Companion and Laguna Insight—conversational AI tools for both care managers and supervisors. Laguna “sits” on top of care management calls and increases efficiency by removing administrative overhead, providing real-time visibility into team performance, and generating actionable insights.
Despite initial reservations about AI potentially diminishing the personal touch in patient care, the team found that Laguna's focus on conversational alliance and empathy actually enhanced the process.
Key stakeholders, including a Registered Nurse and the Director of Case Management, quickly moved from skepticism to advocacy for the new system. They discovered that Laguna didn't replace their roles but instead augmented their ability to provide better care and boosted their productivity.
"The conversational alliance and empathy aspect of Laguna is what makes the platform great. That’s what sets Laguna apart from any other AI vendor.”
—Registered Nurse & Product Manager
The implementation started with a small pilot in late 2024 and, due to its success, rapidly expanded to over 300 users by the spring of 2025.
Results
Increased efficiency and productivity
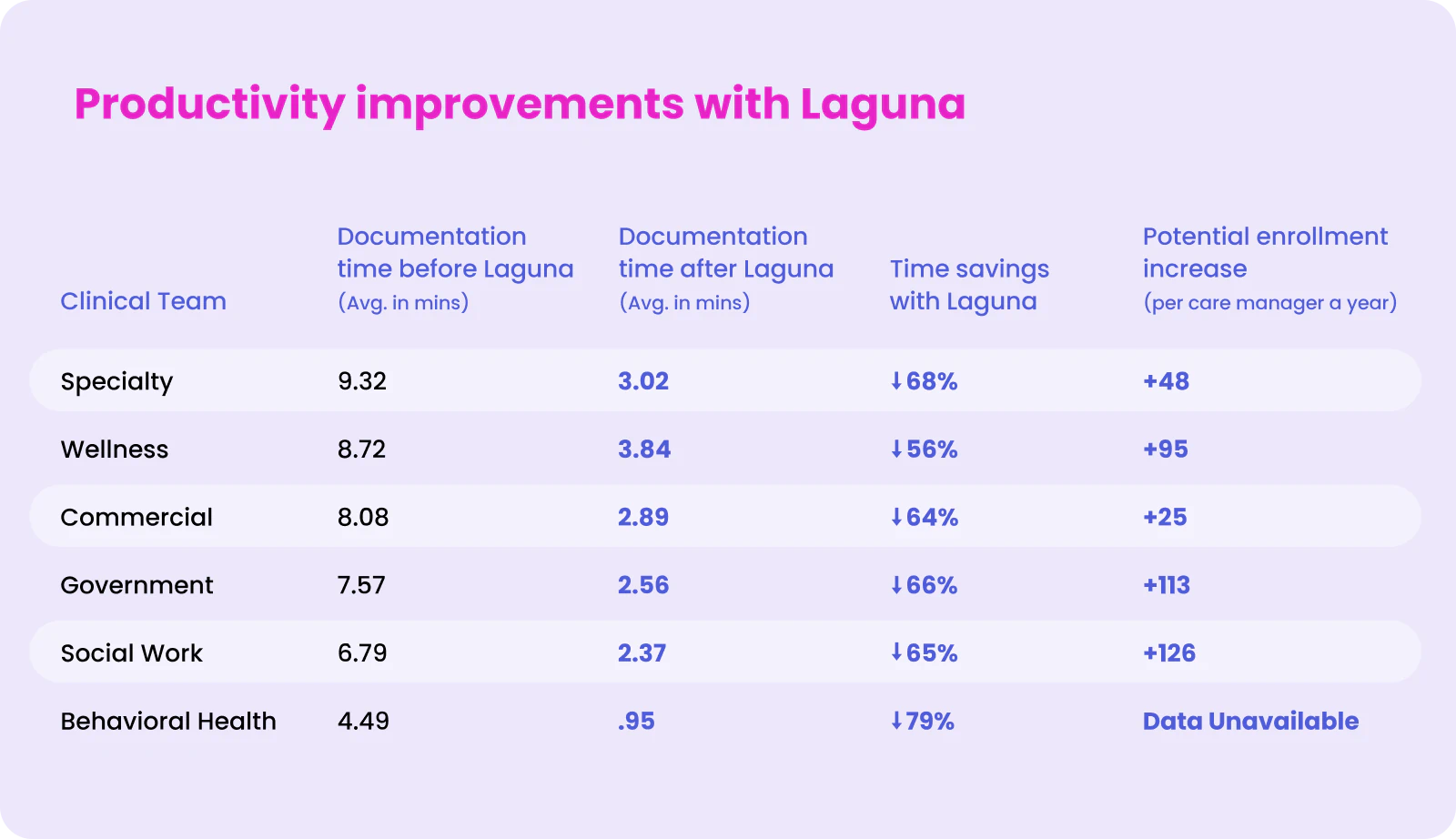
Laguna was able to drive an average of 66% time savings on post-call documentation with very few refinements required, as Laguna has reached a threshold of nearly 100% accuracy in clinical content generated. This in turn results in more time with members and more enrollments into care plans—+96 enrollments per care manager per year on average.
While this was the average time savings demonstrated, it's significant to note that Laguna's ability to tailor documentation by specialty enabled 6 different teams to benefit from those time savings. See the chart below from the health plan's time study demonstrating time savings per team and the estimated increase in enrollment numbers with Laguna.
Improved clinician performance and satisfaction
In addition to efficiency and productivity gains, the leadership emphasized the importance of clinician satisfaction. In surveys with care managers using Laguna, there’s been a significant increase in care manager satisfaction, including:
- 96% of care managers surveyed say they are more efficient with Laguna
- 51% increase in satisfaction with documentation time
- 27% increase in satisfaction with pre-call research
"It's just phenomenal that we have 99% accuracy. As a nurse, you have to trust the results, because it’s your name, your license … They’ve shifted from being a cautious observer to a confident user and for a nurse to do that, that’s a huge step.”
—Director of Case Management


